It’s been a wild ride, where should I start? Bear with me, it’s a long story…

When I first moved to Tampa, I planned on posting multiple days a week, but it’s been an interesting few months. I was able to muster a string of Instagram posts around the holidays in between frequent naps before I knew things would get upended again.
To start, we have to go back to July of 2021 (but we’ll go further back than that in a few!) I had just returned from coming to Tampa for a week to look at apartments, then traveling to LA the following week for my cousin’s wedding, to coming home to start packing my apartment in New York up. I’d gotten an apartment more quickly than I’d planned and needed to move in 2-3 weeks. I was exhausted and stopped my daily Peloton rides and I was avoiding any sort of social interactions because I was so unusually tired.
I got here on August 1 and by the time I’d finished unpacking, decorating my apartment, and getting settled, in between working full-time and a long weekend in September that I was out of town for a friend’s wedding, it was suddenly mid-October. It took me nearly a week to recover from the wedding – and I still didn’t feel rested. My birthday was approaching and I still had zero interest in social gatherings. I was so exhausted but then I couldn’t sleep at night. Days when I could’ve run errands for several hours, I had to come home and lie down after one or two stores. I wasn’t me. I was having gastrointestinal issues, frequent headaches, extreme dry eye, and nerve pain in my leg. So I finally found a doctor and told her what was going on.
I chose this specific doctor because she had excellent reviews for patient care, in women’s health, and for being thorough – but all I got a week later were the results of a standard CBC (complete blood count), a single thyroid test (TSH) and a “prescription” to take vitamins B12 and D until February and then get repeat blood work. I’d asked the doctor to run ferritin because I had low levels in the past that impacted my energy –but she did not. (Ferritin is your iron “reserve” – your iron levels can look fine, but if your ferritin is low, it’s because it’s supplementing your regular iron levels. Having low ferritin can cause a whole host of issues.)
I took the vitamins for a couple of weeks. I had been taking them first thing in the morning with breakfast – until one day I’d forgotten, so I took them after dinner. Within fifteen minutes, I broke out into an intense, itchy hives rash all over my neck and chest and was having trouble breathing. I took a Benadryl and then crushed Benadryl to mix in with instant oatmeal to apply to the rash – but that didn’t work either. I took a Pepcid and found an expired EpiPen in my closet just in case, but the Pepcid did the trick. It turns out, that vitamin B12 has cobalt in it – which I am allergic to. (You might have a cobalt allergy if you are allergic to blue cosmetics, hair dye and some jewelry!) I had been taking Benadryl at night – at the recommendation of my doctor – to sleep and help with the issues I was having with my legs. Because I was taking the Benadryl so late at night, it hadn’t fully metabolized by the time I was taking the B12 in the morning and was keeping me from having an allergic reaction to the cobalt. I had to stop taking the B12 immediately.

By December, I was desperate. About a week before I was set to head to Massachusetts for the holidays, I spent two days only moving between my couch, my bed, and the kitchen. I was so weak and fatigued that I was afraid I was going to fall in the shower and pass out and no one would know, so I didn’t shower and didn’t leave the house. I found a different doctor who had an appointment open the next day and decided to book it, even if I had to Uber to get there.
He checked out my previous blood work before he came into the room and told me he agreed it looked good but asked why I was there. When I told him nothing had resolved, I’d had to stop the B12, and how weak I was, he was immediately concerned. The doctor spent about 45 minutes with me asking a series of questions and taking extensive notes. He asked about my family’s history of autoimmune conditions. We had none. Did I get a rash in the sun? No. What were my gastro symptoms? Awful. How long had all of this been going on? Months. Was I dizzy? Yes. What was my diet like? I could barely eat beyond crackers and popcorn because my stomach was such a mess. He examined me, then offered three options: Do nothing and see how I felt when I returned from Christmas, run additional blood work because he had a few theories, or go to a neurologist to see if there was something else going on.
I chose the blood work and I’m so grateful I did – and so grateful that I chose him for that last-minute appointment before I went home for the holidays.
I ended up with Christmas COVID, like so many people. The worst gift of all. Despite being fully vaccinated and receiving a full third dose in September because of my asthma, I got progressively worse instead of better. I managed to not get my family sick but ended up with a secondary infection that lasted two weeks and had to extend my trip by an extra week because I was so sick that I didn’t feel well enough to travel. In Massachusetts, they were prioritizing unvaccinated people for monoclonal antibodies – despite having a respiratory condition. Paxlovid (the COVID-19 antiviral) had just been approved for EUA by the FDA, so the pharmacies didn’t have it yet. Strangely, during the time I had just COVID-19, it was the most normal I’d felt in months. Fatigue-wise, I had energy during the day and was sleeping again at night. It was borderline frustrating since I was quarantined in my parents’ house and I wanted to go out and do things – but could not.

At the same time, my blood work had come back and it pointed to a potential autoimmune issue. I asked the doctor I’d visited in the 11th hour to become my primary care physician since we hit it off and he’d run tests to point us in a direction. He agreed to take me on and also referred me to a rheumatologist.
By the time I got back to Tampa, my body was about to unleash all of its full hell on me. I had brain fog worse than before my ADHD diagnosis. I couldn’t focus on anything. I felt stupid. Seriously. I couldn’t find simple words to complete sentences. I lost my train of thought frequently. I was even more exhausted than before – and got even less sleep than I was previously – down to 2-3 hours per night. I was forgetting simple things, like inviting other people to meetings. I’d schedule them on my calendar, but never add anyone’s email addresses. I’d never forgotten to do that once in eight months I’d been working at my current job until then, and this was becoming a regular issue. My resting heart rate was often between 115 – 120 bpm (beats per minute) and my eyes were worse than ever. (A regular resting heart rate in healthy people is typically between 60-100 bpm, but can be even lower in athletes. Mine is typically 68-72 bpm.)
My stomach got worse too and I was at the point where I was taking Pepto Bismol almost daily. When I had some energy, I started researching how long my post-COVID symptoms might last and found it could be months and for some, it hadn’t resolved at all. I started taking every supplement and vitamin I could find that people suggested (Collagen, Tumeric, Vitamin D, Glutathione, Iron, Zinc, and a B-Complex). I started taking Nutrafol because my hair was falling out. Then I started taking a probiotic and IBgard. Not much was helping.

When I finally got to the rheumatologist in mid-February, I had been scheduled for an established patient visit, instead of a new patient, which meant I was only scheduled for 15 minutes with the doctor. I’m grateful for him too because he probably wrecked his entire day for me. He stayed with me for nearly an hour taking extensive notes, combing through the existing blood work, and offering me possibilities and potential treatments. He ran a special blood test called AVISE that looks for antibodies for autoimmune disorders and when that came back, I learned I have Hashimoto’s thyroiditis, which is an autoimmune disease that attacks the thyroid gland. I also have an unspecified connective tissue disorder. This explained some of the fatigue and the brain fog, as well as rashes I’d been getting on my neck and chest and intense itching without a rash that caused deep bruising on my legs and arms. While the treatment options included more greens in my diet, hydroxychloroquine, and exercise – the diagnosis didn’t answer the digestive issues or my eye issues. He referred me to a gastroenterologist and an ophthalmologist. I also chose to see an endocrinologist on my own, since thyroid issues run in my family.
Are you sick of these appointments? Me too.
The gastroenterologist turned out to be the key. She didn’t have a straight answer, despite telling me she could usually diagnose by symptoms alone – so we decided on blood work (again) as the first step. Two days after I had the blood drawn, the lab posted my results and I had to Google what Transglutaminase IgA Antibody was. The normal level is 0-15 u/ML … mine was 233.1.
It’s Celiac Disease.
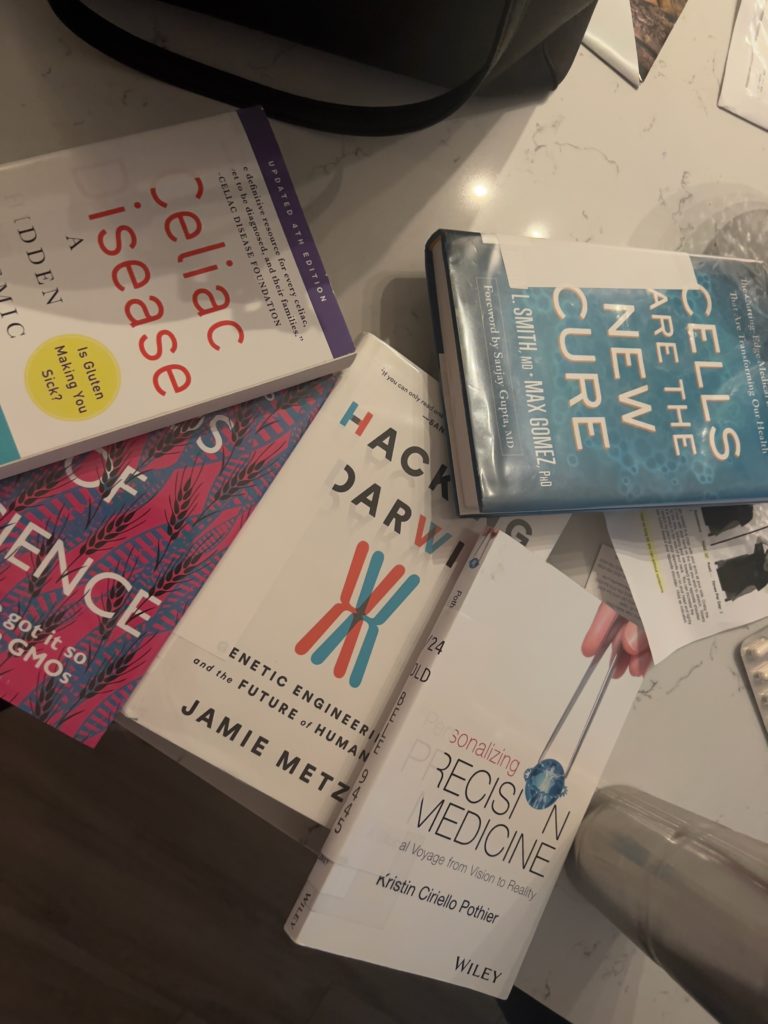
Gluten has been ruining my life and I had no idea. I’ve gone down a research rabbit hole and I’m basically a doctor now (I actually want to figure out how to cure it, no joke – and I’ve watched all 18 seasons of Grey’s Anatomy, so…) and Celiac Disease is a genetic disorder. Most people think it’s just an intolerance or an allergy –but it’s not.
The simplest way to explain it is that gluten-containing foods –wheat, barley, rye, and malt –each have a protein in them that people who have this genetic mutation cannot digest. While most people’s digestive enzymes break down gluten and pass it through their small intestine, my gluten cannot be fully broken down. The fragments sit on top of these finger-like fibers in the small intestine called villi and eventually the body says, ‘Hey, this is an invader! That’s not supposed to be there.’ And it attacks… just like the body attacks a virus when we’re sick. In the process, it damages the villi, inflaming them, and making it even more difficult to digest everything, not just gluten. It causes pain, bloating, and a lot of other not-so-fun side effects. I’ve unknowingly had the gene for Celiac my entire life, but as an autoimmune condition, it can lie dormant in the body until it’s activated by some kind of stressor. Hashimoto’s is the same.
COVID-19 was the stressor.
“But how? You had symptoms last summer, but didn’t have COVID until December!” you’re probably asking.
Well, my doctors and I have traced it back to June/July 2020. I got sick in early May of 2020. It was Nurse’s Week and I was still a broadcast journalist, so I was asked to go talk to our frontline heroes about the work they were doing. It was an important thing to cover and I went to the hospital to do it. It was the only time I left my apartment in two weeks –and we were allowed to walk freely through the ICU. My photographer and I, along with the photographer we’d just hired and were training, were masked – with thin cloth masks. N-95s were still scarce back then for healthcare workers, so I believe the people we were with had surgical masks on at the time. Five days later I woke up with a fever and a cough.
At the time, New York had a lack of tests, a lack of ICU beds, and no ventilators, so we were instructed to stay home for 14 days unless we couldn’t breathe. I was sick, but it was nothing I wasn’t prepared for. I’d been reporting on it for two months, and I was paranoid about getting seriously ill with asthma, so I was ready to do anything necessary to ensure I didn’t get a severe infection. My chest felt like someone was sitting on it, but I forced myself to ride my Peloton every day, used my Albuterol regularly, and laid on my stomach like I’d heard ICU nurses tell me they were doing with their patients. I knew if I couldn’t breathe with my asthma doing all of that, I needed to get treatment, but I didn’t want it to get that far. Most of my symptoms resolved in about a week. Today, I believe it’s because I sweat it out and kept my lungs open so the virus couldn’t fester there and continue to replicate. At the time, I didn’t think much of it and wasn’t even sure it was COVID then because I couldn’t get a test.
By June or July, I noticed that my ADHD medication didn’t seem to be helping me all of a sudden – and I was pretty tired. I was getting regular, itchy rashes on my chest and neck. I consulted my doctor who switched my medication and also put me on a benzodiazepine. “Anxiety hives” was the diagnosis along with “pandemic fatigue.” Everything was still closed and restricted and the pandemic was raging on. She surmised that I was anxious about the pandemic and tired from not only living it but covering it 24/7 as a journalist.

The new medications seemed to help with the focus and fatigue, and the rashes would subside –but I suddenly had gastrointestinal issues and extreme dry eye. These were both potential side effects of my new medications, so I brushed them off.
Now, it all makes sense – this was likely the initial infection that activated my autoimmune conditions. Because we didn’t know some of the long-COVID symptoms yet, or how it might impact us, and I wasn’t even sure I had COVID back then, I just chalked it up to the diagnosis I’d received. Regular office visits weren’t available then – the doctors were doing the best they could via telehealth visits.
In late February 2021, I rushed to get the vaccine as soon as I was eligible. As an asthmatic, I was thrilled to be in the first immunocompromised group in New York. I cried on the way to my appointment, I cried while I was there, I cried on the way home — I was so happy. While I didn’t have a lot of the same side effects most people had, I was exhausted for about two weeks. No fever, no chills, no nausea or vomiting. Just fatigue. When I got my second shot, I felt temporarily better – and then the fatigue came back. That was April 2021.
Then my life got crazy. We’re back to June/July/August 2021, I didn’t think twice about being tired, until I finally got the Celiac results several weeks ago in May 2022.
Celiac Disease not only causes gastrointestinal issues but has an established link to thyroid disorders (they are often co-morbid), along with brain fog, extreme fatigue, a phenomenon called “gluten rash,” which often manifests on the neck and chest, headaches, and dry eye. Oh … and nerve pain and tingling in the legs, which was the very first symptom that prompted me to go to the doctor last October because I was worried about a blood clot. Beyond the damage to the small intestine, because the body cannot digest things properly, Celiacs are also unable to absorb nutrients regularly, which explains all of my low vitamin levels, as well as the fatigue, brain fog, dry eye, and nerve pain.
Ooooof. Are you still with me?!
So, I have an answer. I will either need to avoid gluten altogether or try to avoid it as much as possible, at the present moment – for the rest of my life. It’s a challenge because there is gluten in everything (for example, I bet you didn’t know there is gluten in SOY SAUCE! Yeah.) There are several clinical trials underway and one is in phase 3, but it could still be a few years away if the trial is successful.
I immediately cut gluten out of my diet, purchased supplements to help digest gluten (L-Glutamine and GlutenEase) since my body was still full of it, and upped my intake of probiotics. Within a few weeks, I started to feel like a totally different person –back to how I felt before the pandemic. While I am still adjusting, I have more energy, my stomach is less upset, and I’ve lost 10 pounds without trying. I can only attribute the weight loss to bloat from my body being so inflamed. I can see my cheekbones again; my neck looks slimmer and I no longer look pregnant—which was an ongoing issue for me for several months. I’ve been hiding in yoga pants and loose tops because my weight was only fluctuating by a few pounds and my bloat wasn’t getting better or worse. Now my clothes fit normally again, thank goodness! I think the worst physical manifestation for me was how swollen my face looked. I looked at photos from last year and was shocked to see the difference.







So that’s where I’ve been. I’ve been on a journey that required a lot of advocacy, a lot of research, and one really great doctor who didn’t just tell me to take vitamins, lose weight or exercise more. (Which as women, we are often told to do whenever we have a health problem. And believe me, my Peloton got me through the pandemic mental-health-wise – I was dying to have the energy to work out regularly!) I will eventually share this post with him, and if he is OK with it, add his name here, because he is a fantastic general practitioner.
Now, I get to take the next steps to heal and I get to live normally(ish) again. My family and friends have been supportive – suggesting “gluten-free exploration days,” and checking menus to ensure they’re Celiac-friendly before we pick a place to eat. My mom immediately started Googling for replacements for my favorite items when I was sad. My brand partners have ensured there are gluten-free options for me at events and fellow Celiacs have sent me recipe ideas and options for the best gluten-free options for everything from pizza crust to pasta. I’ve found an incredibly supportive community on Reddit and love the Find Me Gluten Free app. A local restaurant sent me a care package full of swag –but the sweet note they wrote for me was the most touching part. I cried. (And all the Ciccio restaurants in Tampa are fantastic about gluten and cross contamination. I recently went to Daily Eats and the server not only walked me through all the GF options on the menu but made sure to let me know that my home fries were cooked in a special gluten-free only fryer! Anything owned by CRG has been a go-to for me since this diagnosis.)

It’s a journey now that I get to go on, with 1 in every 100 other people who have this genetic disorder, and while the last two months have been challenging, I am just so grateful to have an answer. It boggles my mind that this disease was discovered 2000 years ago – and in modern medicine, was first diagnosed in the 1900s – and yet, in 2022, there is no treatment or cure, other than to switch to a gluten-free diet for the rest of one’s life.
In college, I studied forensic science for the first three years of undergrad, so now I’m using the basics of my background in biology and chemistry. I’m extensively researching Celiac Disease and trying to figure out how I can be part of the solution. Whether that is coming up with an innovative idea (I thought of genetically modifying gluten-containing foods and a “reverse vaccine” to teach the body not to attack the gluten – GMO wheat is already being looked at – and a “reverse vaccine” was fast-tracked by the FDA a few years ago, but ultimately didn’t do well in phase 2 clinical trials and was scrapped. Still, I was glad to know my scientific knowledge from my first three years of college isn’t being wasted!)
I’m also hoping I might qualify to be a participant in a clinical trial, but I’ve decided I do not currently want to get a biopsy to confirm my diagnosis and many of them require this step. My gastroenterologist informed me that before the procedure, I would need to intentionally consume gluten for 4-6 weeks and I do not want to go backward. That being said, I want to be part of improving the quality of life for Celiacs and potentially people with dozens of other autoimmune disorders like diabetes, lupus, MS and so many more. I don’t know what this means for my future, but it is something I am pursuing in my free time for now!
The other thing I am very grateful for is that despite the challenges of this diagnosis, there are people who are suffering far worse consequences from their COVID-19 infections. We know how many people have died, but many who survived and are living with long-COVID syndrome. Some have severe, debilitating, long-term issues and are seeking help from the government to receive disability benefits. Many are unable to do everyday tasks, some lost basic motor skills and some are completely unable to work, care for their families, or even cook their favorite recipes. For a decade or more, we will likely not know the true impacts of COVID – even mild infections – on our bodies. Despite my outcomes, I would still urge everyone who is eligible to receive their COVID-19 vaccines or if you are eligible, the experimental Evusheld monoclonal antibodies meant for those who cannot receive a vaccine. (I recently received Evusheld in lieu of a booster shot at the recommendation of my physician.)
Do you have Celiac or another autoimmune disorder? Please share your experience or tips in the comments. We are on this journey together.